 From the DukeHealth.org archives. Content may be out of date.
From the DukeHealth.org archives. Content may be out of date.
Treating Severe Depression with Electroconvulsive Therapy
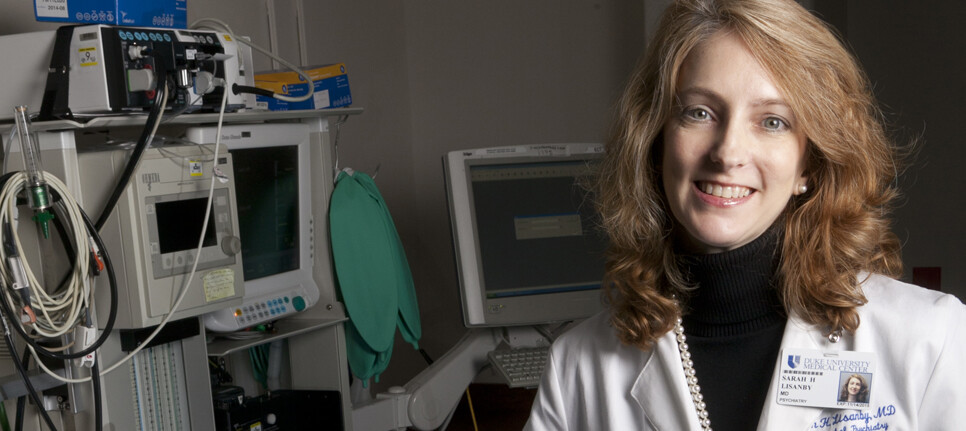
Despite recent advances in treatment, medication-resistant depression continues to impair the lives of thousands each year. Electroconvulsive therapy (ECT) has shown to be the most effective treatment for this devastating disease. Although ECT has been available for many years, modern ECT treatments bear little resemblance to its historical portrayals. Sarah Hollingsworth Lisanby, MD, a geriatric psychiatrist and chair of Duke Department of Psychiatry, discusses the use of ECT to treat depression.
What is ECT?
ECT refers to the most effective and rapidly acting treatment that we have today for severe depression and other conditions, and is used throughout the world.
ECT is an approved medical treatment that involves using electricity to produce a brief seizure in a person under general anesthesia (while the person receiving the treatment is asleep). The seizure usually lasts about a minute or less and body movement is very little because of a strong muscle relaxant medication that is given following the anesthetic drug. ECT is given two to three times per week, usually for six to 12 treatments.
ECT is performed by medical physicians (a psychiatrist and an anesthesiologist), assisted by nurses and other medical staff. ECT is recommended when a severe clinical depression is not responding to other treatments (such as psychotherapy and medications), or when there is a need for a rapid response (such as when there is a high risk of suicide, or the when the depression itself is threatening the health of the person). As such, ECT can be a life-saving treatment because it is rapidly effective, even when other treatments fail.
What Are The Benefits of ECT?
ECT often quickly resolves the symptoms of major depression, including depressed mood, lack of interest, appetite and weight disturbance, sleep disturbance, feelings of hopelessness and helplessness, loss of self esteem, and thoughts of suicide.
Remission, which is the likelihood of having complete resolution of symptoms, is reported to range from 70 to 90 percent with ECT.
ECT is much more effective than any medication we have at present, which typically have remission rates around 20 to 30 percent. ECT can also be used in other conditions when other treatments are not sufficiently effective, such as bipolar disorder, schizophrenia, Parkinson’s disease, and treatment resistant epilepsy.
What Are The Risks of ECT?
Nearly all medical procedures have a risk of side effects. In the case of ECT, the risks relate to the anesthesia and to the seizure.
The risks of anesthesia are relatively low because ECT involves a very brief period of anesthesia, typically lasting less than 10 minutes. Before undergoing ECT, people are evaluated by the anesthesiologist to identify any special risks that anesthesia may pose for them. Unless the person has a very serious medical illness, the risk of life-threatening side effects is extremely rare.
The common risks of the seizure include difficulty with memory (amnesia), as well as temporary headache or muscle aching. The types of memories that can be affected include memories of the past (retrograde amnesia), and the ability to remember new information (anterograde amnesia).
Many patients experience some degree of anterograde amnesia, but this typically disappears soon after the ECT course ends. People receiving ECT can experience varying amounts of retrograde amnesia. Retrograde amnesia typically deals with events that occurred close in time to the ECT, but it can extend further into the past. The amount of memory effect depends to a large extent on the type of ECT received.
Right unilateral ECT (where the right side of the head is stimulated) has less risk of memory loss than bilateral ECT (where the both sides of the head are stimulated). Ultrabrief pulse ECT (which uses a very small amount of electricity) has less risk of memory loss than earlier types of ECT treatment.
Does ECT Damage the Brain?
No. Careful studies using sensitive brain imaging measures in people receiving ECT, and precise anatomical measurements in animal research studies, have repeatedly demonstrated that ECT does not damage the brain.
How Has ECT Been Modernized Over the Years?
Medical advances have dramatically improved ECT, increasing its safety. These advances include general anesthesia, the switch to safer types of electrical stimulation, and the use of right unilateral electrode placement.
When is ECT the Right Treatment?
ECT is indicated for severe clinical depression or bipolar disorder, and other conditions. ECT is typically used when depression is very severe, or has lasted for a long time and not gotten better with psychotherapy and medications.
Sometimes a change in medication dosage, or a switch in medication will be effective for depression, but when it is not, there may be a role for ECT.
Certain types of depression (such as psychotic depression) or catatonic symptoms predict better response to ECT. Older age also predicts better response to ECT.
Is ECT Effective for Older Adults?
There is evidence that older people actually respond better to ECT than those who are younger. The Department of Psychiatry and Behavioral Sciences at Duke is currently investigating the use of ECT in seniors to understand how best to maintain remission after a successful course of ECT.
Currently, relapse is a significant issue for patients who see improvement in their depression after treatment, so this study is important in learning how we can provide long-lasting improvement and prevent relapse in depressed individuals. Effective relapse prevention strategies after ECT are critical to prolonging remission, and that is precisely what we are examining in this study.
For more information or to request an appointment at the Duke Brain Stimulation and Neurophysiology Center, please call 919-681-0603.


