Robot Reduces Need for Open Brain Surgery to Map Epileptic Seizures
A Medical Advance for People with Epilepsy
A robotic device is allowing doctors to pinpoint the origins of a person’s seizures through minimally invasive surgery. The device, in use at Duke and some epilepsy centers across the country, allows neurosurgeons to implant hundreds of recording electrodes into the brain through about 10 to 20 small incisions. The procedure is highly precise, and it takes less time than traditional surgical options for seizure localization. People also recover faster and have less pain.
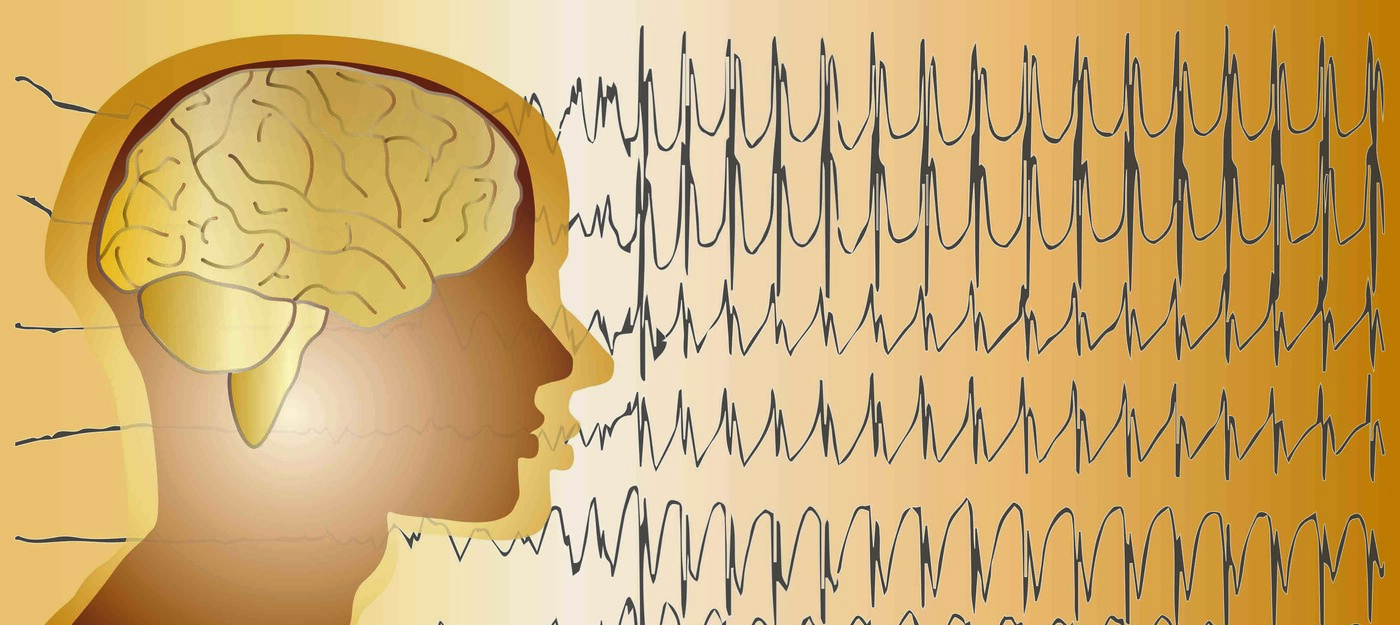
Diagnosing the Origin of Epilepsy Seizures
When medications fail to stop epileptic seizures, a person's best hope for gaining control of their seizures is often epilepsy surgery. That can only happen if doctors can identify the area of the brain responsible for the seizures and remove it safely. To identify that spot, neurosurgeons may perform a craniotomy, creating a large opening in the skull, and then place a plastic grid of electrodes on the surface of the brain to record seizures and identify where they originate. However, the electrodes can’t access the folds or the parts of the brain between the two hemispheres and its deep structures.
Shorter, More Precise Brain Mapping
The team at Duke’s epilepsy center has another tool in their arsenal. Robot-assisted stereoelectroencephalography (SEEG) is a minimally invasive procedure that rapidly places thin electrode wires in precise locations to map the brain and identify seizure origins.
A 3D reconstruction of the brain guides where the dozen or more electrodes will be placed. The neurosurgeon uses a robotic arm to make small, two- or three-millimeter holes in the scalp through which the rigid electrode wire is passed. As opposed to grid electrodes, which sit on the surface of the brain, the wires are placed into the brain tissue with robotic assistance. The procedure takes about two to three hours.
“The robot improves the efficiency of the procedure, and it reduces some of the possibility for human error. Depending on the patient’s condition, robot-assisted SEEG can be very useful for localizing seizures in a way that is more comfortable for patients,” said Duke neurosurgeon Derek Southwell, MD, PhD, of the Duke Comprehensive Epilepsy Center.
Due to its minimally invasive nature, placing depth electrodes this way is much better tolerated by patients than placing grid electrodes. Once the seizure origin is identified, the electrodes are removed, and people recover quickly. That is a huge benefit over recuperating from a craniotomy. The procedure is also better for cases where the exact location of the seizure cannot be identified or the seizure origin is in a part of the brain that is inoperable.