What You Need to Know About Deep Brain Stimulation for Epilepsy
Implanted Device Can Reduce Seizures

Deep brain stimulation (DBS) for epilepsy uses electrical impulses to prevent and reduce seizure severity and frequency, but is it right for you? Here, Duke Health experts answer frequently asked questions to help you decide.
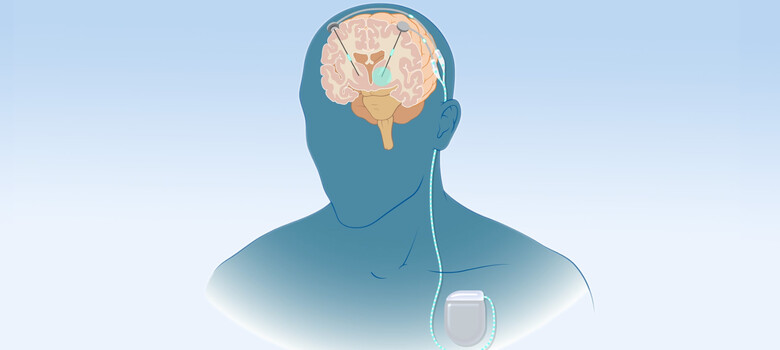
What Is a Deep Brain Stimulator?
A deep brain stimulator is a neuromodulation device made of two parts, said Duke Health neurosurgeon Stephen C. Harward II, MD. The first part consists of electrodes or thin wires that are placed into an area of the brain called the thalamus. The second part is a pulse generator or battery that sends out electrical signals through the electrodes and to the brain. These components are inserted during two separate surgeries, and the device is activated a few weeks after the second procedure.
How Does Deep Brain Stimulation Work?
According to Duke Health epileptologist Birgit Frauscher, MD, deep brain stimulation alters brain circuits to stop seizure activity from spreading or starting. “Your thalamus is like a relay station. When a seizure begins somewhere in the brain, it uses the thalamus as a highway to other areas,” she said. “DBS acts like a roadblock for that kind of travel, and over time, your brain gets better at avoiding it.”
Learn more about how deep brain stimulation works.
Am I a Candidate for DBS for Epilepsy?
You may be a candidate for DBS if you have tried at least two anti-seizure medications without significant improvement and if your seizure focus (the origin of your seizures) is difficult to pinpoint or surgically remove.
At Duke, Dr. Frauscher and her colleagues offer a comprehensive evaluation to determine whether DBS is your best option. This usually requires a stay in our specialized epilepsy monitoring unit at Duke University Hospital. Tests include electroencephalography (EEG) to record brain activity (this may be done using electrodes placed on the scalp and electrodes that are surgically implanted in the brain for up to a week), imaging scans of the brain, and neuropsychological exams to identify cognitive dysfunction or mental health concerns.
“After this testing, our group of epilepsy experts discuss your results and decide whether surgery is right for you,” Dr. Frauscher said. “If we can find your seizure focus and safely remove it, you might be a better candidate for resective surgery. If not, then neuromodulation or specifically DBS may be a good fit.”
When Can I Expect a Benefit? How Much?
Dr. Frauscher said her patients usually start noticing results within a few weeks to months after device activation. Research shows that benefits continue to increase over time, even years later. Many peoples’ seizure frequency is reduced by up to 80%.
Like other neuromodulation devices, DBS requires expert programming to maximize benefit and minimize side effects. Duke’s advanced neuromodulation program is staffed by experts who are experienced in fine-tuning these devices.
What Complications Are Associated with Deep Brain Stimulation?
DBS requires surgery so there is a small risk of bleeding, infection, coma, stroke, or death. The most common side effects of electrical stimulation include tingling, numbness, muscle weakness or muscle contractions, difficulty speaking, eye movement abnormalities, or vision changes. Often these improve by adjusting the DBS device settings. Dr. Frauscher points out that DBS can worsen depression and anxiety.
“It's important to remember that there is risk on both sides. Seizures can lead to injury and even death,” Dr. Frauscher said. “Beyond that, seizures can significantly affect your quality of life, preventing you from driving, working, or doing things you love. So it’s important to weigh all of this.”
Why Should I Choose Duke for Deep Brain Stimulation?
Duke takes a team approach to epilepsy and DBS management. Your care team will include an epileptologist, neurosurgeon, neuropsychologist, and others, which means you benefit from multiple perspectives.
Duke has offered DBS surgery to treat various conditions for 30 years, so our surgical teams have a lot of experience in how to do it safely and effectively, said Dr. Harward. Duke researchers have also been studying and improving this technology for decades. As a result, we can provide the most advanced techniques and approaches. Plus, Duke offers “awake” and “asleep” surgery, meaning you can choose the type of anesthesia you are most comfortable with.
“Duke offers everything you need to be evaluated for DBS therapy, to receive the therapy, and to follow up over time so you get the most benefit from the device,” Dr. Harward said.
What Is My Next Step?
You should seek care at a Level 4 Epilepsy Center like Duke, because those are the only centers that offer DBS in addition to all other available treatment options, according to Dr. Frauscher. “Even if you were evaluated for epilepsy surgery or neuromodulation years ago, we have new tools that weren’t available before but that are highly effective to treat seizures,” she said.
If you haven’t considered neuromodulation before, Dr. Harward said you should talk to your neurologist. “Talking about these treatment options, even years before you might be ready for them, can be very empowering.”