Fertility Preservation Helps Young Breast Cancer Survivor Grow Her Family

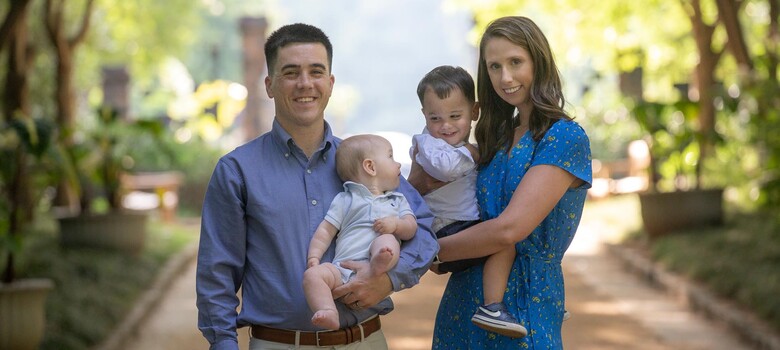
Susan VanNess, 38, enjoys a picnic with her family.
Susan VanNess of Wake Forest was breastfeeding her son when she felt a lump in her breast. She thought it was a cyst or clogged milk duct and made an appointment with her obstetrician. At 38, the mother of two wanted to get pregnant again and figured she could discuss both topics at the visit. When she learned the lump was breast cancer, she was shocked. “I had a one-year-old and my daughter was about to turn four," VanNess said. "Your first thoughts turn to them growing up without a mother.”
After going through her treatment at Duke, VanNess is the proud mom of a new baby girl. "The Duke Cancer Institute saved my life, and I wouldn't be here without them," she said. "I completed my family and my kids get to see me being healthy and happy and appreciating life every day."
Pregnancy-associated Breast Cancer in Young Women
Pregnancy-associated breast cancer, also called gestational breast cancer, occurs during pregnancy or the first post-partum year. While it’s not common, “it is a way that many of our young breast cancer patients present to us,” said Stacy Telloni, MD, a medical oncologist at Duke Women’s Cancer Care Raleigh. Many, like VanNess, think they have a clogged duct.
VanNess Wanted More Children
Within weeks of feeling the lump, VanNess was diagnosed with triple-positive breast cancer, meaning estrogen, progesterone, and a protein called HER2 were fueling her breast cancer cell growth. On February 11, 2021, she underwent a lumpectomy and had seven lymph nodes removed. While they all tested negative for cancer, she needed at least one year of chemotherapy and radiation therapy to ensure the cancer cells were destroyed. That was concerning, she said, because “I wanted to have one more child.”
Timing Fertility Preservation
“Fertility preservation is definitely a topic of concern for my young breast cancer patients,” said Dr. Telloni. Cancer treatment like chemotherapy can damage the ovaries. “It can put women into early menopause.”
Since her chemotherapy had to start soon, Dr. Telloni referred VanNess to the Duke Fertility Center. VanNess started in vitro fertilization (IVF) about a week after her lumpectomy to produce embryos for her doctors to harvest and freeze for a future pregnancy. “We typically advise patients to wait two years from diagnosis before becoming pregnant,” Dr. Telloni said.
Cold Cap Therapy Can Prevent, Reduce Hair Loss from Chemotherapy
About one month after IVF, VanNess started her weekly chemotherapy regimen at Duke Women’s Cancer Care Raleigh. With her sister’s help, she used cold cap therapy, which required placing -40-degree dry ice on her scalp on chemotherapy days to reduce hair loss.
According to Dr. Telloni, cold cap therapy theoretically works by constricting the blood vessels in the scalp, which protects the hair follicles. “Cooling caps can prevent or reduce hair loss from chemotherapy,” she said. “Susan was on weekly chemotherapy. Cold capping took some effort, but it worked. Susan lost very little hair.”
Duke Women’s Cancer Care Raleigh Offers Many Services
Duke Women’s Cancer Care Raleigh offers many services to its patients including physical therapy exercises and massages to help manage lymphedema, scar tissue, mobility issues, and pain. A dietician is available to discuss dietary concerns such as nausea, appetite loss, and taste change. A medical family therapist helps families cope with the trauma of a loved one going through cancer, and a sexual health therapist helps people come to terms with the physical and psychological changes that result from treatment. People can continue to use these services once their cancer treatment is over.
Expanding Family as a Cancer Survivor
Today, VanNess is one of many cancer survivors receiving ongoing treatment at Duke Women’s Cancer Care Raleigh. She’s on hormone therapy to prevent cancer from returning and sees her oncologist every six months. "I now have a baby girl who is only a month old," she said. "She wouldn't be here if it wasn't for my doctor and the care team at Duke listening to me and tailoring my program."
VanNess also said cancer has made her understand what’s important in life. “Cancer can be a blessing in this weird way. You find out who your support system truly is when you’re going through a really difficult time. You no longer take for granted the mundane things you took for granted in the past.”
For Dr. Telloni, working with cancer patients like VanNess is the essence of why she does what she does. “One of the best things about my job is watching patients become survivors, especially young people like Susan. And it’s been amazing to see several of my patients have children.”